
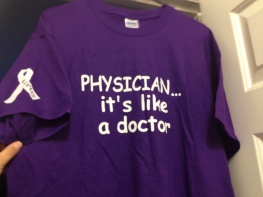
It made my day today when my doctor walked in and pointed out he was wearing not one but two purple shirts for Lupus Awareness! One of them being a shirt we made for him! I wish I could have gotten a picture of him in it, but I at least have a picture of the shirt from before we gave it to him. There is a story behind it and hopefully he won’t mind me telling it on here. My friend Penny and I ran into him one day at lunch and were chatting with him when the waiter happened by and asked him what he did for a living. He replied “I’m a Family Physician at HFP”. The waiter looked at him and then asked, “Is that like a doctor?” Dr. C replied “Yes it is exactly like a doctor”. After the waiter returned inside much laughter ensued. It was rather amusing. After I told my husband the story, being the screen-printer he is, it quickly because a shirt slogan and I gave it to Dr. C at my next INR check.
Today was a follow-up appointment with him. This appointment was on the books a month ago and was supposed to be the appointment where we talked about the fact I had started Imuran and caught up on notes from my last Rheumatology appointment. Since I started Imuran ahead of schedule we didn’t have to do that part. For the most part we have already seen the impact it is going to have on my INR and warfarin dose. For me it appears very little impact is occurring. One this I did forget to mention at my appointment and I will make a note to tell Dr. C next time is that this is absolutely the max dose of Imuran I’ll be on because of how my test results came back when Dr. L tested how I metabolize Imuran. That is the one piece of information I forgot to mention today.
I did tell Dr. C that Monday’s appointment overwhelmed me, left me in tears, and that it was like a completely different doctor had walked into my appointment than the Dr. L I had met at my previous appointment. I told him about Dr. L’s sudden change of mind that we really need to track down the antibodies to prove Lupus and that it caught me off guard a good deal. I showed him the information on the Dermatologist that Dr. L wants me to see for the skin biopsies. We talked it over and he is leaving it up to me unless it comes down to Dr. L requiring me to have them done to continue treatment. I showed him the codes that were on my paperwork that I had to give to the checkout lady at Dr. L’s office and he was able to explain what the medical codes meant. I was correct that the first code meant Undifferentiated Connective Tissue Disease and the other two codes were apparently just reminder codes to my insurance company that I am on high risk medications (Imuran & Warfarin). With that being said, he did tell me that both himself, Dr. M and of course myself still all believe this is Lupus. He reminded me that Dr. L is one of the older doctors, so his Dr. M but not all of the older doctors are stuck into the older way of diagnosing Lupus. I told him that I had learned through looking at my medical records from Dr. L that my ssDNA (single strand DNA antibodies) were moderately high when his lab tested me for Lupus a few weeks ago. The problem with this antibody is that I A) didn’t test positive enough for their likings and B) it is not specific to SLE. It CAN show up with Drug induced Lupus, Rheumatoid Arthritis and Chronic Hepatitis. Today we discussed that we are pretty sure I don’t have Hepatitis (We have had many conversations over liver issues because my aunt died from Autoimmune Hepatitis and I am terrified of liver issues now), my Rheumatoid Factor does not support a diagnosis of RA. I am on one drug that can sometimes cause drug-induced Lupus. Here’s the thing though, at the time of the test, I had not been on it for very long, certainly not long enough to cause DI-Lupus AND all of my symptoms predate the start of Lisinopril. So we are again pretty sure this is SLE. I also have anticardiolipin antibodies, which is part of my Antiphospholipid Syndrome, the blood clotting disorder. However, this antibody is pretty common in Lupus patients that also have APS. Confused yet? Yep my medical conditions overwhelm me and cause me to research and ask lots of questions.
So where we stand today is much like I said earlier in the week, It’s still Lupus. We are treating it and hopefully things will slowly start to improve as we continue to do so. Speaking of treatments I told him I thought one of the things that upset Dr. L was that I hadn’t been taking Naproxen as he had instructed me to do between appointments. The thing is I’ve had conversations with both Dr. C and my Hematologist, Dr. M and both of them have in the past laid out the risks of taking Naproxen while on Warfarin. So I’ve erred on the side of caution and used the methods that Dr. C and I have figured out worked for me. I have a topical gel that he prescribed that does wonders when my joints start swelling and it has the benefit of being an NSAID that I can apply directly to the afflicted joint and it’s not systemic so I don’t get the interaction with Warfarin that I get when I start taking Naproxen. I also have a pain med that Dr. C prescribed and when the pain gets too bad I take it. The truth is most days I just deal with the pain because I hate taking pain meds. Even when I need them I hate taking them. I’ve spoken of my dad’s drug issues in the past, just knowing what his addictions did to him cause me to question if I should even get near pain meds. I know there is very little risk in me becoming an addict, I don’t have an addictive personality, unless you count my scarf obsession, my yarn collection, or silly things like that. Still they make me nervous so I don’t take them unless I need them. The last time Dr. C called in a prescription for Tramadol he gave me two refills, I have yet to use the first refill. I still have most of the first prescription left. Granted we ended up having to do a round of steroids in the midst of all this but even those aren’t a long-term option to fixing my pain. Luckily though Dr. C is understanding where I come from with my issues with pain meds. I explained to him the deal with Naproxen and that Dr. L wants me to start taking it at the rate of 1-2 in the mornings and 1-2 in the evenings and that he seemed upset that I hadn’t adhered to this treatment plan. I told him that Dr. L had also said that he has plenty of patients on both meds that have no problems. We both agreed that he probably does, but perhaps none of them have Dr. M telling them not to take Nsaids. I do have a follow-up with Dr. M coming up at the beginning of June so I will also talk to him about all of this then as well.
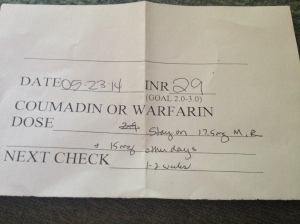 We also checked my INR at this appointment. It has been 10 days since my last INR check. We had been doing it every week but recently Dr. C said we could start spacing them every 1-2 weeks. I’m not comfortable enough yet to go the full two weeks so I’m splitting it up and going every 10 days for now. I also want to Dr. M about this before I go making too many changes to the frequency of my INR checks. I figure if I’m going to have a Hematologist I should ask him these sort of questions. Today my INR was 2.9. My goal range is 3-3.5(ish). We don’t tend to freak out if it’s a little over. We decided to leave my dose the same because I’m pretty sure the dip is due to this stress induced flare I have brought upon myself this week. Word of caution, stress is not good for folks with autoimmune conditions. It tends to cause a flare in their symptoms. For me it has caused a flare in my joint pain and fatigue and a small dip in my INR. The really cool thing about this dip in my INR, was even though it was lower than we want it to be it didn’t dip me into the range that causes me to have major issues with my APS. Until recently my INR was still in a range where if it dipped it was dipping low enough I would have transient clotting events, dizziness, migraines. This time, it was comforting to see that even with this flare the dip took me just below my target range, and that was still high in the therapeutic range which means clots are of very low risk! Next week I have therapy with AL on Tuesday, then my next INR check and the labs Dr. L is having Dr. C run for him are on 6/2, Dr. M is 6/9.
We also checked my INR at this appointment. It has been 10 days since my last INR check. We had been doing it every week but recently Dr. C said we could start spacing them every 1-2 weeks. I’m not comfortable enough yet to go the full two weeks so I’m splitting it up and going every 10 days for now. I also want to Dr. M about this before I go making too many changes to the frequency of my INR checks. I figure if I’m going to have a Hematologist I should ask him these sort of questions. Today my INR was 2.9. My goal range is 3-3.5(ish). We don’t tend to freak out if it’s a little over. We decided to leave my dose the same because I’m pretty sure the dip is due to this stress induced flare I have brought upon myself this week. Word of caution, stress is not good for folks with autoimmune conditions. It tends to cause a flare in their symptoms. For me it has caused a flare in my joint pain and fatigue and a small dip in my INR. The really cool thing about this dip in my INR, was even though it was lower than we want it to be it didn’t dip me into the range that causes me to have major issues with my APS. Until recently my INR was still in a range where if it dipped it was dipping low enough I would have transient clotting events, dizziness, migraines. This time, it was comforting to see that even with this flare the dip took me just below my target range, and that was still high in the therapeutic range which means clots are of very low risk! Next week I have therapy with AL on Tuesday, then my next INR check and the labs Dr. L is having Dr. C run for him are on 6/2, Dr. M is 6/9.
Overall it was a good appointment. He was able to reassure me and remind me that I still have some control in this insane situation. Plus he wore Purple! Yes he is that awesome! He has another patient that has Lupus and it is sweet that he is showing support for us. Not many doctors would have gone this extra step. It was a small act that says I care! That goes a long way and I hope he realizes how much that means to me.
I remember going to school with you! It’s great the way you have become a writer and informing the public.
LikeLike
Thanks Michael! I was glad I figured out it was you! 🙂 Also glad you are finding my blog informative.
LikeLike
He sounds great!
LikeLike
He is! I am blessed to have him as my main doctor!
LikeLike
I am ready for bed now and am wearing a purple dressing-gown! I read your post and it seems you are on an incredible journey. Your doctor sounds wonderful. Sending you good wishes for all good things now and in your future, Nicole. 😊
LikeLike